Articles
- Page Path
- HOME > J Liver Cancer > Volume 24(1); 2024 > Article
-
Original Article
Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study -
Kazuya Kariyama1
 , Kazuhiro Nouso1
, Kazuhiro Nouso1 , Atsushi Hiraoka2
, Atsushi Hiraoka2 , Hidenori Toyoda3
, Hidenori Toyoda3 , Toshifumi Tada4
, Toshifumi Tada4 , Kunihiko Tsuji5
, Kunihiko Tsuji5 , Toru Ishikawa6
, Toru Ishikawa6 , Takeshi Hatanaka7
, Takeshi Hatanaka7 , Ei Itobayashi8
, Ei Itobayashi8 , Koichi Takaguchi9
, Koichi Takaguchi9 , Akemi Tsutsui9
, Akemi Tsutsui9 , Atsushi Naganuma10
, Atsushi Naganuma10 , Satoshi Yasuda3
, Satoshi Yasuda3 , Satoru Kakizaki11
, Satoru Kakizaki11 , Akiko Wakuta1
, Akiko Wakuta1 , Shohei Shiota1
, Shohei Shiota1 , Masatoshi Kudo12
, Masatoshi Kudo12 , Takashi Kumada13
, Takashi Kumada13
-
Journal of Liver Cancer 2023;24(1):71-80.
DOI: https://doi.org/10.17998/jlc.2023.09.11
Published online: November 6, 2023
1Department of Gastroenterology, Okayama City Civic Hospital, Okayama, Japan
2Gastroenterology Center, Ehime Prefectural Central Hospital, Matsuyama, Japan
3Department of Gastroenterology and Hepatology, Ogaki Municipal Hospital, Ogaki, Japan
4Department of Internal Medicine, Japanese Red Cross Society Himeji Hospital, Himeji, Japan
5Center of Gastroenterology, Teine Keijinkai Hospital, Sapporo, Japan
6Department of Gastroenterology, Saiseikai Niigata Hospital, Niigata, Japan
7Department of Gastroenterology, Gunma Saiseikai Maebashi Hospital, Maebashi, Japan
8Department of Gastroenterology, Asahi General Hospital, Asahi, Japan
9Department of Hepatology, Kagawa Prefectural Central Hospital, Takamatsu, Japan
10Department of Gastroenterology, National Hospital Organization Takasaki General Medical Center, Takasaki, Japan
11Department of Clinical Research, National Hospital Organization Takasaki General Medical Center, Takasaki, Japan
12Department of Gastroenterology and Hepatology, Kindai University Faculty of Medicine, Higashiosaka, Japan
13Department of Nursing, Gifu Kyōritsu University, Ogaki, Japan
-
Corresponding author: Kazuhiro Nouso, Department of Gastroenterology, Okayama City Civic Hospital, 3-20-1 Kitanagase-Omotemachi, Kita-ku, Okayama 700-8557, Japan
Tel. +81-86-737-3000, Fax. +81-86-737-3019 E-mail: kazunouso@gmail.com
© 2024 The Korean Liver Cancer Association.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 954 Views
- 93 Downloads
- 3 Citations
Abstract
-
Background/Aim
- The aim of this study was to compare the therapeutic efficacy of ablation and surgery in solitary hepatocellular carcinoma (HCC) measuring ≤5 cm with a large HCC cohort database.
-
Methods
- The study included consecutive 2,067 patients with solitary HCC who were treated with either ablation (n=1,248) or surgery (n=819). Th e patients were divided into three groups based on the tumor size and compared the outcomes of the two therapies using propensity score matching.
-
Results
- No significant difference in recurrence-free survival (RFS) or overall survival (OS) was found between surgery and ablation groups for tumors measuring ≤2 cm or >2 cm but ≤3 cm. For tumors measuring >3 cm but ≤5 cm, RFS was significantly better with surgery than with ablation (3.6 and 2.0 years, respectively, P=0.0297). However, no significant difference in OS was found between surgery and ablation in this group (6.7 and 6.0 years, respectively, P=0.668).
-
Conclusion
- The study suggests that surgery and ablation can be equally used as a treatment for solitary HCC no more than 3 cm in diameter. For HCCs measuring 3-5 cm, the OS was not different between therapies; thus, ablation and less invasive therapy can be considered a treatment option; however, special caution should be taken to prevent recurrence.
- Molecular targeting agent therapies, including tyrosine kinase inhibitors and immune checkpoint inhibitors, have been developed in recent years for the treatment of unresectable advanced hepatocellular carcinomas (HCCs), and their use is a subject of debate.1-7 On the contrary, surgery or local ablation is still the recommended treatment for early-stage HCCs of three nodules or less that are ≤3 cm in size. However, several studies have suggested that surgery may be superior to ablation in terms of overall survival (OS) and recurrence-free survival (RFS).8-11 A study also indicated that surgery is superior in terms of RFS, even if the OS is the same.12 Some studies have also found that surgery is superior to ablation for HCCs measuring >2 cm.10 Conversely, no significant difference in OS and RFS was found between surgery and ablation in patients with solitary lesion measuring ≤3 cm.13,14 The debate continues to this day, and the results of a recent prospective randomized controlled study, the SURF trial, conducted in Japan for early-stage HCCs of three nodules or less that are ≤3 cm in size and a Child-Pugh score of ≤7 showed no significant difference in progression-free survival (PFS) between surgery and ablation.15 Based on the result of this study, the Japanese Society of Hepatology guideline for 2021 recommends both surgery and local ablation for HCCs of three nodules or less that are ≤3 cm in size.16 However, 90% of the HCC cases enrolled in the SURF trial were solitary HCCs.15 In addition, the mean tumor diameter in the SURF trial was 1.8 cm, and the 75th percentile tumor diameter was 2.3 cm, which may not provide sufficient evidence to consider treatment options for HCC measuring 2-3 cm in actual clinical practice.
- Recently, there has been a heated debate over the choice between surgery and ablation for a solitary HCC measuring >3 cm but <5 cm.8,12,16,17 Ng et al.8 demonstrated that ablation is not significantly different from surgery in terms of OS and RFS for single HCCs measuring ≤5 cm in diameter. Conversely, in a retrospective study, Zheng et al.13 found that surgery was superior to ablation for HCCs measuring >3 cm and ≤5 cm in terms of both OS and RFS. Additionally, Lee et al.18 conducted a randomized controlled trial and found that surgery was significantly superior to ablation for HCCs measuring >2 cm and ≤4 cm. These studies do not provide a consensus on the efficacy of ablation for HCCs measuring >3 cm and ≤5 cm, and further research is needed in this area. Therefore, we conducted a retrospective study using the large database of the RELPEC Study Group to investigate the prognostic value of ablation in HCCs measuring ≤5 cm, including HCCs measuring >3 cm and ≤5 cm.
INTRODUCTION
- Patients
- We analyzed 2,067 consecutive patients from the RELPEC Study Group who had undergone ablation (including combination with transarterial chemoembolization) or surgery for a solitary HCC with a maximum diameter of ≤5 cm as the first-line therapy. These patients were enrolled from 2004 (when reimbursement for radiofrequency ablation [RFA] was approved in Japan) to 2020. In terms of surgery, out of 819 cases, 582 (71%) underwent open liver resection, while 237 (29%) underwent laparoscopic liver resection. HCC diagnosis was established using imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and angiography. The diagnostic criteria for HCCs were based on previous reports of hyperattenuation in the arterial phase and hypoattenuation in the portal phase as determined by dynamic CT or MRI with tumor staining on angiography.19 The diagnosis was confirmed pathologically in cases with atypical findings using tissues obtained from a fine-needle tumor biopsy. The tumor, node, and metastasis staging for HCCs was determined based on the 6th edition of the general rules for the clinical and pathological study of primary liver cancer developed by the Liver Cancer Study Group of Japan.20
- The study protocol complied with the ethical guidelines of the World Medical Association Declaration of Helsinki and was approved by the ethics committee of the institutional review board (IRB) of Ehime Prefectural Central Hospital (approval code: 27-34), and we had permission to use our multi-institution data.
- Propensity score matching (PSM) and prognostic analysis
- The patients were divided into three groups based on tumor size, which are ≤2 cm, >2 cm but <3 cm, and >3 cm but <5 cm. A propensity score was obtained using surgery as the objective variable and age, sex, viral/non-viral carcinogenesis, albuminbilirubin (ALBI) score, log alpha-fetoprotein, log des-gammacarboxy prothrombin, and tumor size as explanatory variables. The obtained propensity scores were used for matching, with a caliper of 0.2, using caliper matching. As regards caliper width, Austin's recommendation of 0.2 was adopted.21 The OS and RFS were evaluated in each group before and after the matching.
- Statistics
- Data were expressed as median and range. All statistical analyses were performed using Easy R (Saitama Medical Center, Saitama; Jichi Medical University, Shimotsuke, Japan),22 a graphical user interface for R (The R Foundation, Vienna, Austria).23 Prognostic analysis was performed using PSM, the Kaplan-Meier method, the log-rank test and Cox proportional hazard model.
METHODS
- Patients
- Patient characteristics are shown in Table 1. Significant differences in age, sex, ALBI score, platelet count, prothrombin time, albumin, aspartate transaminase, total bilirubin, and Des-γcarboxy prothrombin were found between the surgery and ablation groups. In the group with tumors ≤2 cm in size, 271 surgeries and 844 ablations were performed. In the group with tumors >2 cm but ≤3 cm in size, 232 surgeries and 320 ablations were performed. In the group with tumors >3 cm but ≤5 cm in size, 316 surgeries and 84 ablations were performed.
- PSM and prognostic analysis
- OS and RFS were examined before and after PSM.
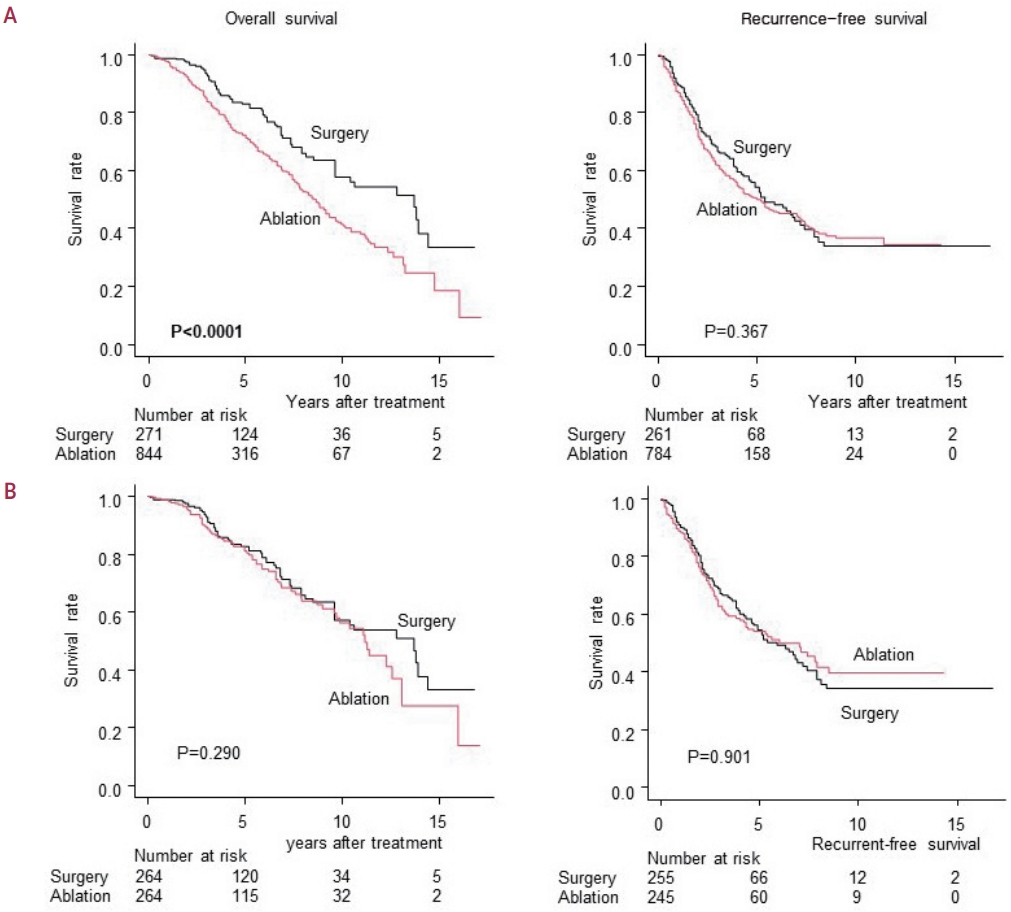
- Before PSM, the surgery group had significantly better OS (P<0.0001); however, the RFS was not significantly different between the surgery and ablation groups (P=0.367) (Fig. 1A). PSM was performed, and 528 cases (264 in each group) were extracted. No significant differences were found between the two groups in terms of age, sex, viral/non-viral status, ALBI score, log alpha-fetoprotein, log des-gamma-carboxy prothrombin, and tumor size in the background factors of surgery and ablation cases after PSM (Table 2). No significant difference was found in the OS after PSM between the surgery and ablation groups (13.7 years [95% confidence interval (CI), 9.6-14.4] vs. 11.2 years [95% CI, 9.6-13.1]; mean observation period, 5.1 years; P=0.290). No significant difference in RFS was found (5.9 years [95% CI, 4.6-7.4] vs. 6.0 years [95% CI, 4.2-8.5]; mean observation period, 3.5 years; P=0.901) (Fig. 1B).
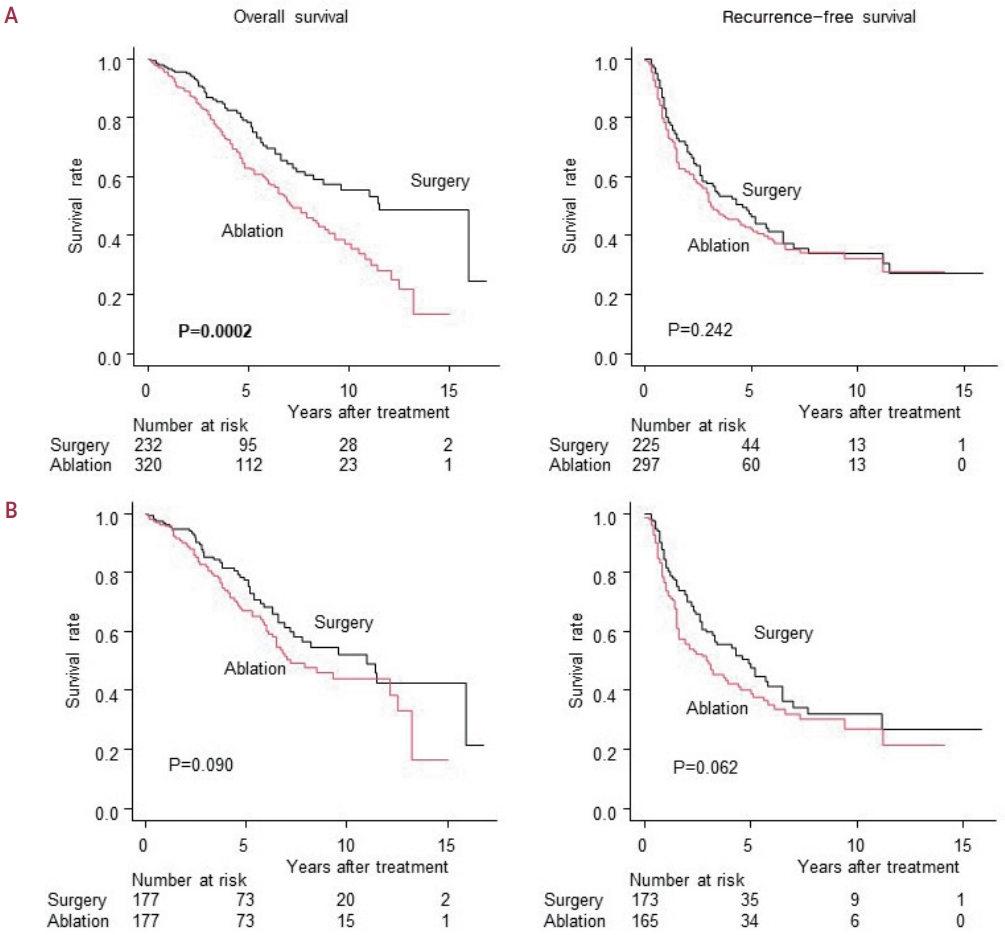
- The OS before PSM was significantly better in the surgery group (P=0.0002), but no significant difference in RFS was found between the surgery and ablation groups (11.0 years [95% CI, 7.2-not reached] vs. 7.2 years [95% CI, 6.1-12.5]; mean observation period, 4.7 years; P=0.242) (Fig. 2A). PSM was then performed on 354 cases (177 cases in each group). After matching, only the viral/non-viral background of the liver could not be matched, and this difference was significant (P=0.043) (Table 3). The OS after PSM was not significantly different between the surgery and ablation groups (P=0.090). Moreover, no significant difference in RFS was found between the two groups (4.9 years [95% CI, 3.2-6.5] vs. 3.0 years [95% CI, 1.6-4.4]; mean observation period, 2.9 years; P=0.062) (Fig. 2B).
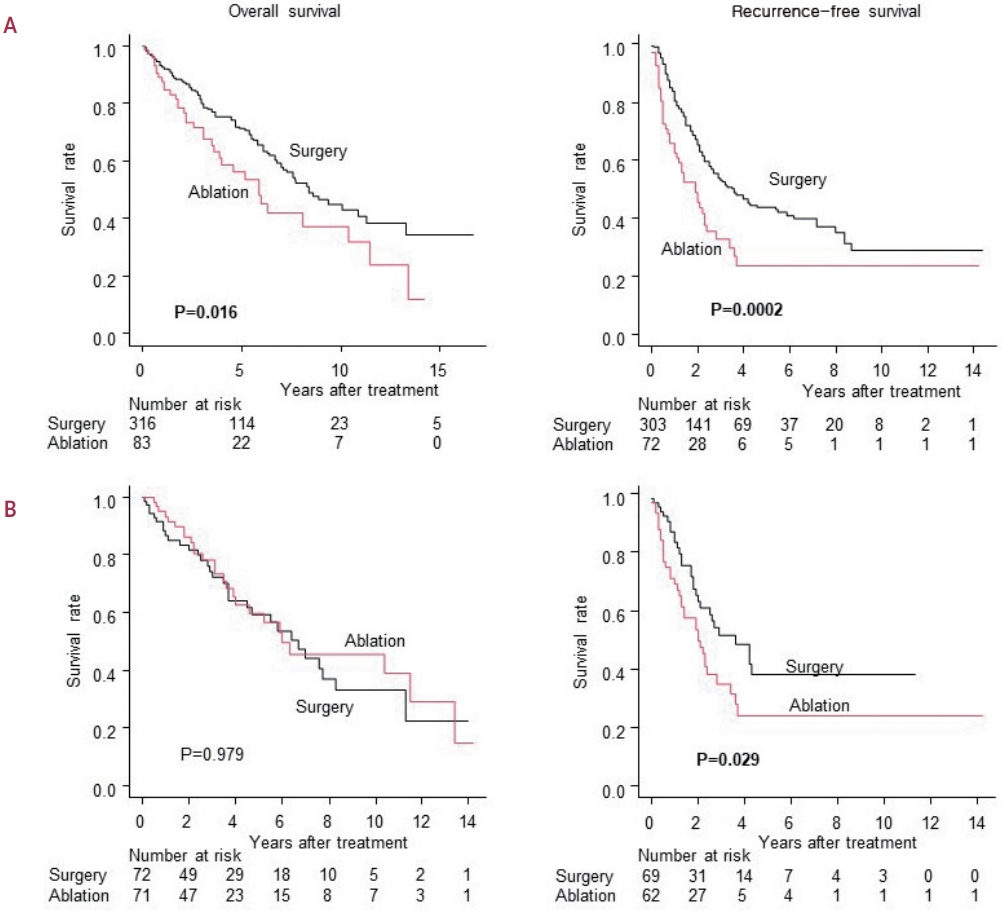
- Before PSM, both the OS and RFS were better in the surgery group (P=0.016 and P=0.0003, respectively) (Fig. 3A). For PSM, 144 patients (72 in each group) were selected. After matching, no significant differences in background factors were found between the groups (Table 4). After PSM, the significant difference in OS between surgery and ablation disappeared (6.7 years [95% CI, 3.7-8.3] vs. 6.0 years [95% CI, 3.9-13.4]; mean observation period, 3.4 years; P=0.979), but RFS remained significantly better in surgery (3.7 years [95% CI, 2.0-not reached] vs. 2.0 years [95% CI, 1.3-2.8]; mean observation period, 2.5 years; P=0.029) (Fig. 3B).
- The hazard ratios before and after PSM for OS/RFS in ablation surgery compared to surgery are shown in Table 5. Consistent with the results obtained from Kaplan-Meier analysis, no significant difference was observed between ablation and surgery in terms of OS after PSM. However, for RFS, surgery remained significantly superior to ablation even after PSM.
RESULTS
Group with tumor size ≤2 cm
Group with tumor size >2 cm but ≤3 cm
Group with tumor size >3cm but ≤5 cm
Summary of hazard ratio before and after PSM in OS and RFS of ablation compared to surgery
- This retrospective study found that when background factors were matched by PSM, no significant difference in the OS and PFS was found between surgery and ablation in patients with a single HCC measuring ≤2 cm. In addition, the OS and PFS were not different between surgery and ablation in patients with RFS of HCCs measuring >2 cm to 3 cm or less, suggesting that patients with a single HCC measuring ≤3 cm can confidently be recommended for ablation. On the contrary, the PFS was shorter in the ablation group than in the surgery group when the HCC size was >3 cm but <5 cm, although the OS of both groups was the same.
- In multiple randomized controlled studies, including the SURF trial,8,15,18 surgery and ablation are equivalent for tumors measuring ≤3 cm. However, many of these reports include numerous cases with single tumors measuring ≤2 cm, where the efficacy of RFA has already been established. More than half of HCCs in the SURF trial was ≤2 cm, and no studies have focused on HCCs measuring >2 cm and <3 cm. Our study addressed this gap and demonstrated the efficacy of ablation for tumors of this size.
- While surgery showed better RFS than ablation for solitary HCC measuring >3 cm but <5 cm, the same level of OS can be achieved through ablation, which is a less invasive option. In older patients, and when considering minimally invasive approaches, treatment must be selected carefully, particularly considering the risk for post-treatment adverse events.24 In a randomized controlled trial of ablation and surgery, Chen et al.24 reported that major complications after treatment occurred significantly more frequently after surgery than after ablation (50 of 90 patients in the resection group and 3 of 71 patients in the ablation group, P<0.05). Additionally, all patients had moderate/severe pain after surgery, whereas only 16 patients required pain medication after percutaneous local ablation therapy (P<0.05).24 In older patients with HCC, treatment-associated complications are an important factor in treatment selection, even if surgery is superior in terms of RFS. If the OS is the same, ablation can be considered a viable option.
- In actual clinical practice, the primary reasons for performing ablation in cases with tumor diameter exceeding 3 cm are 1) patients declining hepatectomy, 2) inability to perform hepatectomy due to compromised liver reserve, and 3) inability to undergo hepatectomy due to poor performance status caused by factors such as advanced age. Thus, the choice between hepatectomy and ablation is not solely determined by the tumor size, but rather depends on the individual patient's condition. Wang et al.25 stated that for the treatment of HCC measuring 3-5 cm, microwave ablation therapy, even when compared to the minimally invasive treatment of laparoscopic hepatectomy, demonstrates equivalent overall survival and complication rates. Additionally, the hospitalization period is significantly shorter, and medical expenses are lower.25 This report also underscores the importance of ablation, emphasizing the need to consider it as one of the treatment options in the future.
- While Japanese and Korean guidelines do not recommend ablation for HCCs measuring >3 cm,14,26 Taiwanese guidelines recommend ablation even for solitary HCC measuring <5 cm,27 and our study supports this recommendation. Our study demonstrates the effectiveness of ablation for solitary HCC that is between 3 cm and 5 cm in size. However, the success of ablation may vary at different medical centers. Special techniques, such as artificial ascites and pleural effusion, may be required to ensure the success of the ablation and minimize the risk of complications from the ablation affecting nearby organs.
- Zhang et al.11 examined a large number of solitary HCC as we did in the present study and concluded that surgery was superior both in OS and RFS for HCCs measuring >3 cm and ≤5 cm. A possible reason for this inferiority of ablation is shorter OS and RFS in the ablation group than in our study because of the low successful ablation rate. However, we cannot know the exact reason because they only showed hazard ratios and did not present the survival rates or additional details. By contrast, the current study clearly demonstrated the lack of a significant difference in OS between surgery and ablation for solitary HCC measuring >3 cm and ≤5 cm, using Kaplan-Meier analysis. Therapeutic support of ablation such as fusion images, artificial ascites, and pleural effusion was routinely used in the present study.28-32 Those supports are known to increase the success rate of ablation so that the survival rate of ablation in the present study must be higher than that in the former and is comparable to that of resection.28-32
- This study has several limitations, including its retrospective nature, conducted only in Japan, multicenter setting, and varying treatment strategies among centers.
- Nevertheless, this study clearly demonstrated the effectiveness of the ablation for the treatment of solitary HCC measuring 2-3 cm and <2 cm. In addition to HCCs measuring <3 cm, ablation can be used for the treatment of 3-5 cm HCC, especially for the treatment of older patients because of its low invasiveness, although special caution should be taken to prevent recurrence in these cases. Prospective randomized controlled studies, especially for single HCCs measuring 3-5 cm, are desirable.
DISCUSSION
-
Conflict of Interest
Kazuhiro Nouso is an editorial board member of Journal of Liver Cancer, and was not involved in the review process of this article. Otherwise, the authors have no conflicts of interest to disclose.
-
Ethics Statement
The study protocol conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki and was approved by our Ehime Prefectural Central Hospital Institutional Review Board (IRB No. 27-34). All procedures were done in accordance with the Declaration of Helsinki. The need for written informed consent was waived because of the retrospective nature of the study.
-
Funding Statement
This research received no external funding.
-
Data Availability
The data, analytical methods, and research materials used in this study are not available to other researchers.
-
Author Contribution
Conceptualization: KK, TK
Data curation: AH, HT, TT, KT, TI, EI, TH, KT, AT, SY, SK, AW, SS, TK
Methodology: TK
Writing-original draft: KK
Writing-review & editing: KN, MK
Article information
Acknowledgments
Values are presented as median (range) or number (%).
C, hepatitis C virus; B, hepatitis B virus; Alc, alcohol; NBNC, non-B and non-C; ALBI score, albumin-bilirubin score; AST, aspartate transaminase; ALT, alanine transaminase; AFP, alpha fetoprotein; AFP-L3, lens culimaris agglutinin-reactive AFP isoform; DCP, des-γ-carboxy prothrombin.
- 1. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378−390.ArticlePubMed
- 2. Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 2018;391:1163−1173.ArticlePubMed
- 3. Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebocontrolled, phase 3 trial. Lancet 2017;389:56−66.ArticlePubMed
- 4. Zhu AX, Kang YK, Yen CJ, Finn RS, Galle PR, Llovet JM, et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 2019;20:282−296.ArticlePubMed
- 5. Abou-Alfa GK, Meyer T, Cheng AL, El-Khoueiry AB, Rimassa L, Ryoo BY, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med 2018;379:54−63.ArticlePubMedPMC
- 6. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 2020;382:1894−1905.ArticlePubMed
- 7. Kelley RK, Sangro B, Harris W, Ikeda M, Okusaka T, Kang YK, et al. Safety, efficacy, and pharmacodynamics of tremelimumab plus durvalumab for patients with unresectable hepatocellular carcinoma: randomized expansion of a phase I/II study. J Clin Oncol 2021;39:2991−3001.ArticlePubMedPMC
- 8. Ng KKC, Chok KSH, Chan ACY, Cheung TT, Wong TCL, Fung JYY, et al. Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg 2017;104:1775−1784.ArticlePubMedPDF
- 9. Hsiao CY, Hu RH, Ho CM, Wu YM, Lee PH, Ho MC. Surgical resection versus radiofrequency ablation for Barcelona Clinic Liver Cancer very early stage hepatocellular carcinoma: long-term results of a singlecenter study. Am J Surg 2020;220:958−964.ArticlePubMed
- 10. Imai K, Beppu T, Chikamoto A, Doi K, Okabe H, Hayashi H, et al. Comparison between hepatic resection and radiofrequency ablation as firstline treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res 2013;43:853−864.ArticlePubMed
- 11. Zhang T, Hu H, Jia Y, Gao Y, Hao F, Wu J, et al. Efficacy and safety of radiofrequency ablation and surgery for hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Medicine (Baltimore) 2022;101:e32470.ArticlePubMedPMC
- 12. Ivanics T, Rajendran L, Abreu PA, Claasen MPAW, Shwaartz C, Patel MS, et al. Long-term outcomes of ablation, liver resection, and liver transplant as first-line treatment for solitary HCC of 3 cm or less using an intention-to-treat analysis: a retrospective cohort study. Ann Med Surg (Lond) 2022;77:103645. ArticlePubMedPMC
- 13. Zheng L, Zhang CH, Lin JY, Song CL, Qi XL, Luo M. Comparative effectiveness of radiofrequency ablation vs. surgical resection for patients with solitary hepatocellular carcinoma smaller than 5 cm. Front Oncol 2020;10:399. ArticlePubMedPMC
- 14. Ko SE, Lee MW, Ahn S, Rhim H, Kang TW, Song KD, et al. Laparoscopic hepatic resection versus laparoscopic radiofrequency ablation for subcapsular hepatocellular carcinomas smaller than 3 cm: analysis of treatment outcomes using propensity score matching. Korean J Radiol 2022;23:615−624.ArticlePubMedPMCPDF
- 15. Takayama T, Hasegawa K, Izumi N, Kudo M, Shimada M, Yamanaka N, et al. Surgery versus radiofrequency ablation for small hepatocellular carcinoma: a randomized controlled trial (SURF trial). Liver Cancer 2021;11:209−218.ArticlePubMedPMCPDF
- 16. Kudo M, Kawamura Y, Hasegawa K, Tateishi R, Kariyama K, Shiina S, et al. Management of hepatocellular carcinoma in Japan: JSH consensus statements and recommendations 2021 update. Liver Cancer 2021;10:181−223.ArticlePubMedPMCPDF
- 17. Thamtorawat S, Hicks RM, Yu J, Siripongsakun S, Lin WC, Raman SS, et al. Preliminary outcome of microwave ablation of hepatocellular carcinoma: breaking the 3-cm barrier? J Vasc Interv Radiol 2016;27:623−630.ArticlePubMed
- 18. Lee HW, Lee JM, Yoon JH, Kim YJ, Park JW, Park SJ, et al. A prospective randomized study comparing radiofrequency ablation and hepatic resection for hepatocellular carcinoma. Ann Surg Treat Res 2018;94:74−82.ArticlePubMedPMCPDF
- 19. Kudo M, Kitano M, Sakurai T, Nishida N. General rules for the clinical and pathological study of primary liver cancer, nationwide follow-up survey and clinical practice guidelines: the outstanding achievements of the Liver Cancer Study Group of Japan. Dig Dis 2015;33:765−770.ArticlePubMedPDF
- 20. Liver Cancer Study Group of Japan. The general rules for the clinical and pathological study of primary liver cancer, 6th ed. Tokyo: Kanehara, 2015:26-30.
- 21. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 2011;10:150−161.ArticlePubMedPMCPDF
- 22. Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013;48:452−458.ArticlePubMedPMCPDF
- 23. R Core Team. The R project for statistical computing, 2023 [Internet]. Vienna (AT): R Foundation for Statistical Computing; [cited 2023 Aug 5]. Available from: https://www.R-project.org/
- 24. Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 2006;243:321−328.ArticlePubMedPMC
- 25. Wang Z, Liu M, Zhang DZ, Wu SS, Hong ZX, He GB, et al. Microwave ablation versus laparoscopic resection as first-line therapy for solitary 3-5- cm HCC. Hepatology 2022;76:66−77.ArticlePubMedPDF
- 26. Korean Liver Cancer Association (KLCA), National Cancer Center (NCC) Korea. 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. Clin Mol Hepatol 2022;28:583−705.ArticlePubMedPMCPDF
- 27. Shao YY, Wang SY, Lin SM; Diagnosis Group, Systemic Therapy Group. Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J Formos Med Assoc 2021;120:1051−1060.ArticlePubMed
- 28. Minami Y, Kudo M. Image guidance in ablation for hepatocellular carcinoma: contrast-enhanced ultrasound and fusion imaging. Front Oncol 2021;11:593636. ArticlePubMedPMC
- 29. Minami Y, Minami T, Hagiwara S, Ida H, Ueshima K, Nishida N, et al. Ultrasound-ultrasound image overlay fusion improves real-time control of radiofrequency ablation margin in the treatment of hepatocellular carcinoma. Eur Radiol 2018;28:1986−1993.ArticlePubMedPDF
- 30. Nishimura M, Nouso K, Kariyama K, Wakuta A, Kishida M, Wada N, et al. Safety and efficacy of radiofrequency ablation with artificial ascites for hepatocellular carcinoma. Acta Med Okayama 2012;66:279−284.PubMed
- 31. Uehara T, Hirooka M, Ishida K, Hiraoka A, Kumagi T, Kisaka Y, et al. Percutaneous ultrasound-guided radiofrequency ablation of hepatocellular carcinoma with artificially induced pleural effusion and ascites. J Gastroenterol 2007;42:306−311.ArticlePubMedPDF
- 32. Kariyama K, Nouso K, Wakuta A, Kishida M, Nishimura M, Wada N, et al. Percutaneous radiofrequency ablation for treatment of hepatocellular carcinoma in the caudate lobe. AJR Am J Roentgenol 2011;197:W571−W575.ArticlePubMed
References
Figure & Data
References
Citations

- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Kazuhiro Nouso, Kazuya Kariyama
Journal of Liver Cancer.2024; 24(1): 5. CrossRef - Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
Ji Hoon Kim, Pil Soo Sung
Journal of Liver Cancer.2024; 24(1): 1. CrossRef - Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Jongman Kim
Journal of Liver Cancer.2024; 24(1): 3. CrossRef
 PubReader
PubReader ePub Link
ePub Link Download Citation
Download Citation
- Download Citation
- Close
- Related articles
-
- Current perspectives on radiotherapy in hepatocellular carcinoma management: a comprehensive review
- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
- Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
- The efficacy of treatment for hepatocellular carcinoma in elderly patients
- Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study

 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION



 Follow JLC on Twitter
Follow JLC on Twitter