Articles
- Page Path
- HOME > J Liver Cancer > Volume 21(1); 2021 > Article
-
Original Article
Incidence and Clinical Features of Hepatitis C Virus-associated Hepatocellular Carcinoma Patients without Liver Cirrhosis in Hepatitis B Virus-endemic Area - Jongbeom Shin, Jung Hwan Yu, Young-Joo Jin, Jin-Woo Lee
-
Journal of Liver Cancer 2021;21(1):34-44.
DOI: https://doi.org/10.17998/jlc.21.1.34
Published online: March 31, 2021
Division of Gastroenterology, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Korea
-
Corresponding author: Young-Joo Jin, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, 27 Inhang-ro, Jung-gu, Incheon 22332, Korea,
Tel. +82-32-890-2548, Fax. +82-32-890-2549, E-mail; jyj412@hanmail.net, https://orcid.org/0000-0002-7449-2461 - * These two authors are co-first authors who equally contributed to this work.
Copyright © 2021 by The Korean Liver Cancer Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,130 Views
- 90 Downloads
- 1 Citation
Abstract
-
Background/objective
- Hepatitis C virus (HCV)-associated hepatocellular carcinoma (HCC) is rarely observed in patients without liver cirrhosis (LC). We evaluated the incidence and clinical feature of HCV-associated HCC patients with or without LC.
-
Methods
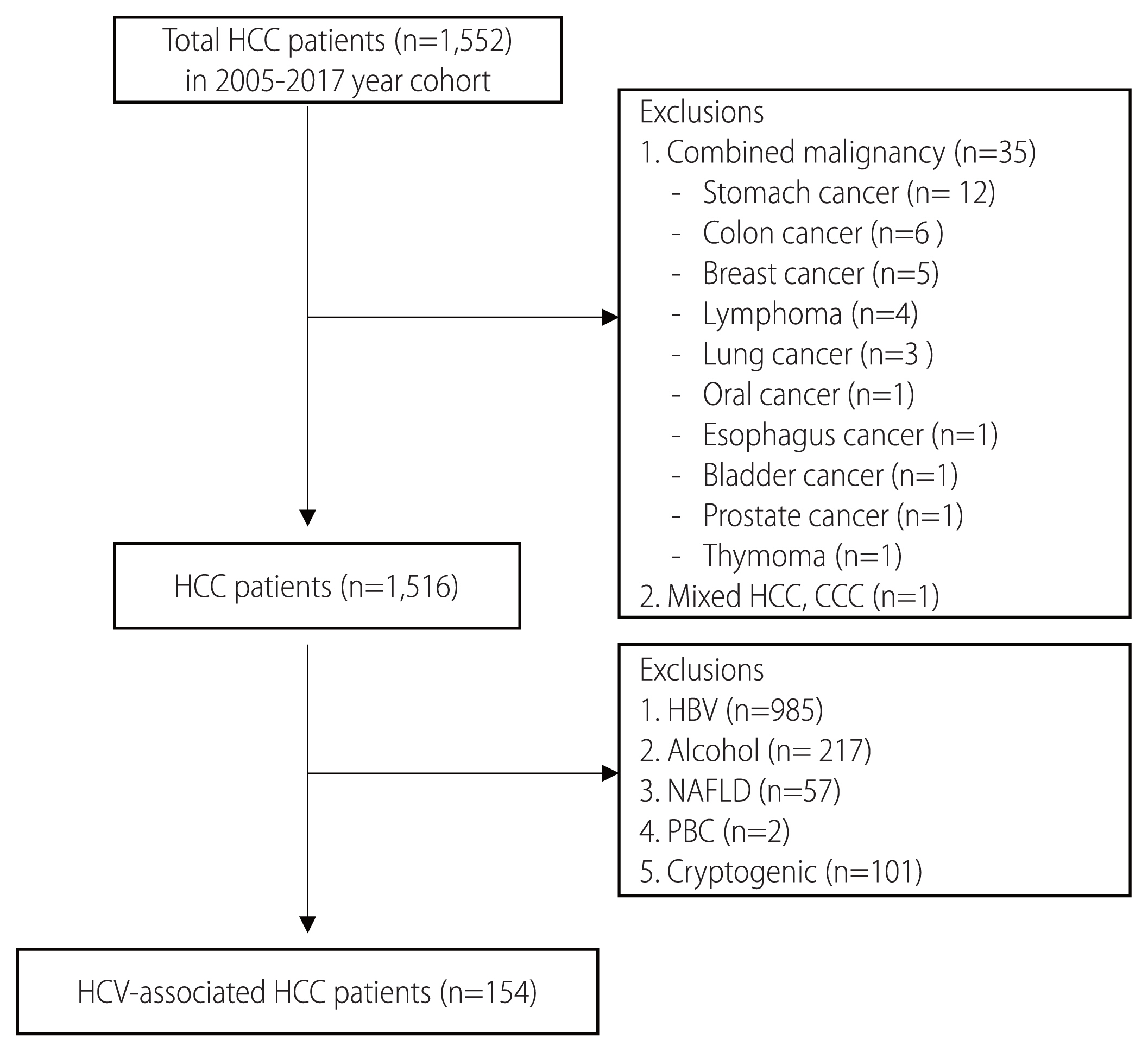
- The medical records of 1,516 patients diagnosed as having primary HCC at our hospital between January 2005 and December 2017 were retrospectively reviewed. Of these, 154 (10.2%) HCV-associated HCC patients were analyzed. LC was diagnosed histologically or clinically.
-
Results
- Seventeen (11.0%) of the 154 patients had non-cirrhotic HCC, and all were of Child-Turcotte-Pugh (CTP) class A, Among the 17 patients, 88.2% were male, all had nodular type HCC, and only 2 (11.8%) were under HCC surveillance. Median overall survival (OS) of HCV-associated HCC patients with and without LC was 15 months and 37 months, respectively. Cumulative OS rates were not different between non-cirrhotic patients and cirrhotic patients with CTP class A (P=0.229). Cumulative OS rates were significantly higher in non-cirrhotic patients than in cirrhotic patients of CTP class B (P<0.001) or C (P<0.001). Multivariate analyses showed serum AST (hazard ratio [HR] 1.01, P=0.003) and AFP levels (HR 1.01, P=0.016), antiviral therapy (HR 0.25, P=0.022), and LC of CTP class B (HR, 5.24, P=0.006) or C (HR 21.79, P<0.001) were significantly associated with prognosis in HCV-associated HCC patients.
-
Conclusions
- HCC in a non-cirrhotic liver was found in 11% of HCV-associated HCC patients. OSs of HCV-associated HCC patients were better in those of CTP A, regardless of LC than in those with LC of CTP class B or C.
- Hepatocellular carcinoma (HCC) is the sixth most common human cancer and the fourth in terms of cancer-related global mortality.1 Underlying liver cirrhosis (LC) is the main risk factor for HCC development regardless of underlying liver disease.2 However, not all HCC patients have LC, and HCCs have been reported to develop occasionally in non-cirrhotic livers.3–5 Among Asian hepatitis B virus (HBV) carriers without LC, HCC risk remains high regardless of HBV replication status.6–8 On the other hand, HCC development in hepatitis C virus (HCV) patients without LC has not been clearly defined, although the risk of HCC in chronic HCV patients with LC has been well established.9,10
- In HCV patients with LC, the annual incidence of HCC is known to range between 2% and 8%,10,11 but the risk of HCC development in HCV patients without LC has been reported to be much lower.12,13 In a previous study, the 5-year risk of HCC development in HCV patients without LC was reported to be 4.8%.12 Recently, more HCV patients than ever have received oral direct acting antiviral (DAA) therapy for chronic HCV infection. And, the risks of persistent chronic inflammation and progression to cirrhosis in these patients is expected to reduced.14,15 Nonetheless, the occurrence of HCC was not reduced in HCV patients with LC treated with DAA.16 Moreover, recent studies have reported HCC risk does not fully disappear in HCV patients without LC even after the achievement of sustained virologic response (SVR) on antiviral therapy (AVT) for chronic HCV infection.17–19 However, these studies were conducted in Western countries, where HCV is the main etiology of HCC.17–19 Although two recent studies analyzed the risks of HCC in HCV patients on AVT in HBV endemic areas,20,21 these studies were conducted only on patients being treated on AVT for HCV and did not assess the clinical features of HCC in HCV patients without LC. Moreover, the proportion of HCV-associated HCC patients without underlying LC among all HCC patients has not been well defined in HBV-endemic areas, and the clinical features of these patients remain to be determined.
- In this cross-sectional and longitudinal study, therefore, we retrospectively compared the incidences and clinical features of HCV-associated HCC patients with or without LC residing in an HBV-endemic area. In addition, we also evaluated the overall survivals (OSs) of these patients according to the Child-Turcotte Pugh (CTP) classification.
INTRODUCTION
- 1. Study subjects
- Between January 2005 and December 2017, 1,552 patients were initially diagnosed with HCC at our hospital. Patients with a treatment history of HCC at other institutions before visiting our hospital were not enrolled. HCC was diagnosed based on the American Association for the Study of Liver Diseases (AASLD) guidelines.22 Of these 1,552 patients, 36 patients with another combined malignancy or mixed type of HCC with cholangiocarcinoma were excluded (Fig. 1). Of the 1,516 HCC patients without another combined malignancy, 1,362 patients with HBV (n=985), alcohol-related HCC (n=217), non-alcoholic fatty liver disease (n=57), primary biliary cirrhosis (n=2), or cryptogenic disease (n=101) were also excluded (Fig. 1). The 154 (154/1,516, 10.2%) remaining HCV-related HCC patients were retrospectively enrolled in this study. All had been anti-HCV antibody positive for at least 6 months at enrollment. LC was diagnosed based on histologic findings, or clinically according to the presence of portal hypertension (HTN) (encephalopathy, esophageal varices, ascites, or splenomegaly, or a low (<100,000/mm3) platelet count),23 or radiologically according to ultrasonographic, computed tomographic, or magnetic resonance imaging (MRI) findings,24,25 or based on aspartate aminotransferase (AST) to platelet ratio index (APRI) or fibrosis index based on four factors (FIB-4).26,27
- At diagnosis of HCV-associated HCC, HCC patients were divided into two groups, that is, into HCCs that developed in a non-cirrhotic (non-cirrhotic group) and cirrhotic liver background (cirrhotic group), and their cross-sectional data were obtained. These patients were regularly followed up every 3 to 6 months by serum alpha-fetoprotein (AFP) measurement and ultrasonography (USG) or computed tomography, 28 and their longitudinal data were collected. Diabetes mellitus (DM) (type 2) was defined as a previous diagnosis or the taking of relevant medications at enrollment, and HTN was defined as a systolic blood pressure of ≥ 130 mmHg or taking relevant drugs at enrollment.29 This study was approved by the Institutional Review Board of Inha University Hospital, Incheon, South Korea (INHAUH 2017-11-017-002).
- 2. Statistical Analyses
- Clinical variables of study subjects are presented as medians (ranges) for continuous variables, and as numbers (percentages) for categorical variables. The chi-square test, Fisher’s exact test, or the Student’s t-test were used to determine the significances of difference between categorical or continuous variables. Kaplan-Meier analysis and the log-rank test were used to analysis survival outcomes. In multivariate analyses, hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated by Cox proportional hazards regression analysis to identify predictors of OS. These predictors were evaluated at time of initial HCC diagnosis, and clinical factors, such as, age, gender, body mass index (BMI), presence of DM or HTN, AST, alanine aminotransferase (ALT), CTP class, tumor number, size, and type, AFP, and Barcelona Clinical Liver Cancer (BCLC) stages were included in the analysis. SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA) was used throughout, and two-tailed P-values of <0.05 were considered statistically significant.
METHODS
- 1. Baseline characteristics of the study subjects
- Baseline clinical characteristics of the 154 study subjects are shown in Table 1. Of the 1,516 primary HCC patients without other combined malignancies, 154 (10.2%) patients were diagnosed as having HCV-associated HCC (Fig. 1). Of these 154 patients, 17 (11.0%) were the non-cirrhotic group, and 137 (89.0%) were the cirrhotic group (Table 1). Median age of the 154 study subjects was 66 years (range, 41–87 years), and 99 (64.3%) were male. Median BMI was 24.2 kg/m2 (range, 13.8–43.3 kg/m2), and DM and HTN were present in 58 (37.7%) and 66 (42.9%), respectively. One hundred three (66.9%) of the study subjects were of CTP class A, and 22 (14.3%) had experience of antiviral treatment (AVT). Almost all (n=149, 96.8%) patients had nodular type HCC, and 86 (55.8%) had a single HCC. Median tumor size was 2.7 cm (range, 1.0–16.0 cm), and 94 (61.0%) patients had HCC of BCLC stage 0 or A. Thirty (19.5%) patients underwent treatment with curative-intent, that is, surgical resection (n=12) or radiofrequency ablation (n=18). Overall median follow-up duration was 18.0 months (range, 1–142 months). Between the cirrhotic and non-cirrhotic groups, the proportion of males (P =0.032) or CTP class A (P =0.004), median platelet count (P <0.001), and median albumin level (P <0.001) were significantly higher in the non-cirrhotic group. Median follow-up duration was longer in the non-cirrhotic group (P =0.019), but median BMI, AST, ALT, total bilirubin, prothrombin time (PT), and AFP levels were significantly lower in the non-cirrhotic group (all P-values< 0.05). A history of AVT for HCV infection before diagnosis of HCV-associated HCC and tumor characteristics were not significantly different in the two study groups (all P-values>0.05).
- 2. Clinical features of HCV-associated HCC without LC
- In order to identify the clinical features of patients in the non-cirrhotic group, 17 HCV-associated HCC cases without LC were individually assessed (Table 2). Median age in this group was 68 years (range 46–85 years), and 15 were male. Platelet counts were over 100 (×103/uL) in all patietns. Only two (11.8%) of the 17 patients had a history of AVT for HCV infection, and the AVT regimen used was interferon-based. However, these two patients did not achieve SVR. In addition, two (11.8%) of the 17 patients had been under HCC surveillance using USG with serum AFP. However, in these two patients, USG was performed annually, not every 6 months, and serum AFP levels were low (2.9 and 13.1 ng/mL, respectively). At diagnosis of HCC, these two patients had no initial symptoms. With regard to tumor characteristics, 10 had a single and 7 had two HCC(s), and median tumor size was 4.2 cm (range, 2.1–8.3 cm). In one of the 17 patients, HCC exhibited portal vein thrombosis (PVT) by tumor invasion, and 10 had HCC within Milan criteria. Twelve, four, and one of the 17 patients had HCCs with BCLC stages A, B, and C, respectively. Interestingly, in case 5, the patient was diagnosed as having HCC with BCLC stage B despite a history of AVT and annual HCC surveillance.
- 3. OS rates of HCV-associated HCC patients according to the presence of LC
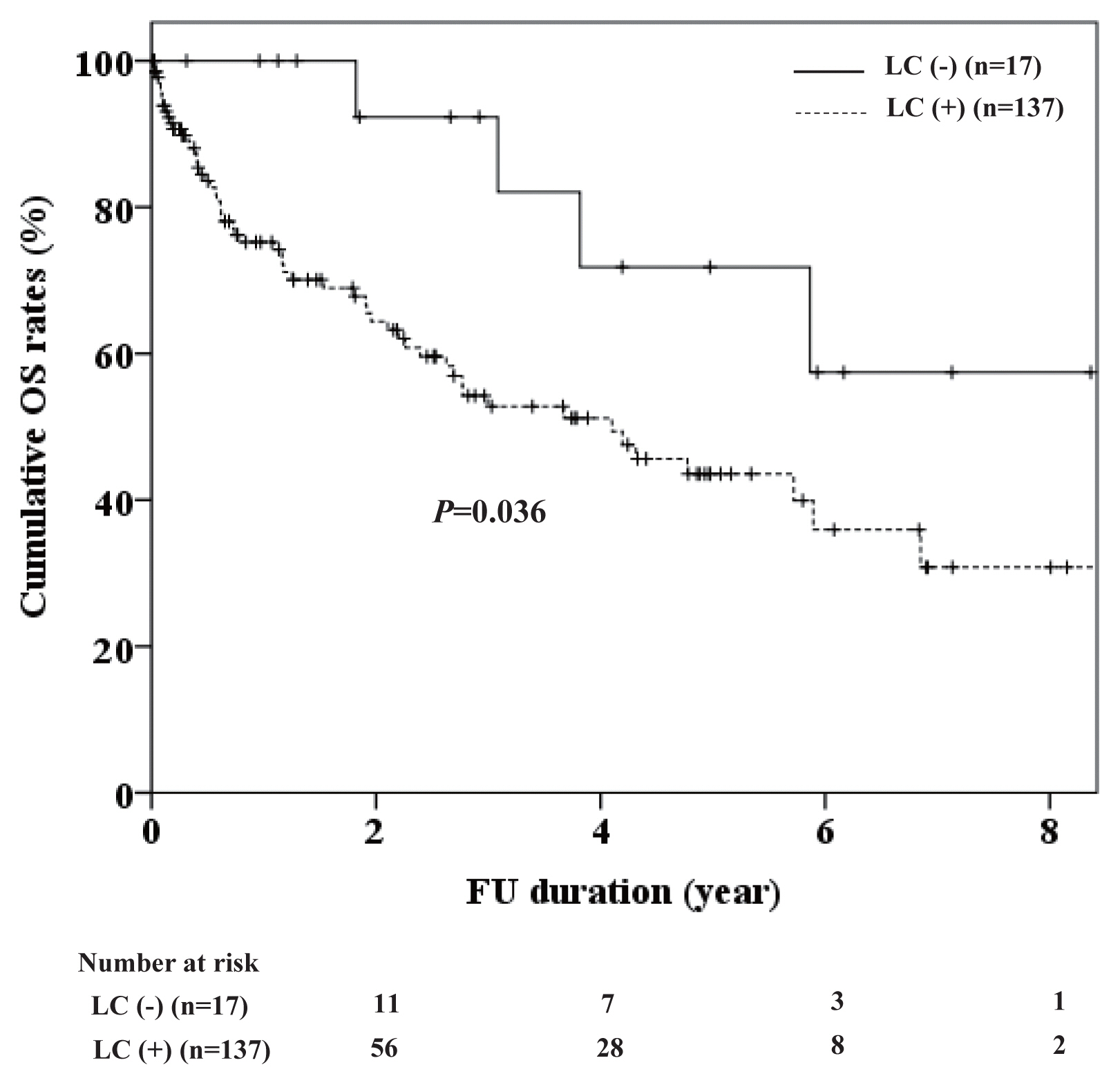
- During the follow-up period, 4 of the 17 non-cirrhotic patients died, and 57 of the 137 cirrhotic patients. Median OSs of HCV-associated HCC patients with and without LC were 15 months and 37 months, respectively. The 2-, 4-, and 6-year cumulative OS rates of the non-cirrhotic group were 92.3%, 71.8%, and 57.4%, respectively. And, the 2-, 4-, and 6-year cumulative OS rates of the cirrhotic group were 64.4%, 51.2%, and 35.9%, respectively (P = 0.036) (Fig. 2).
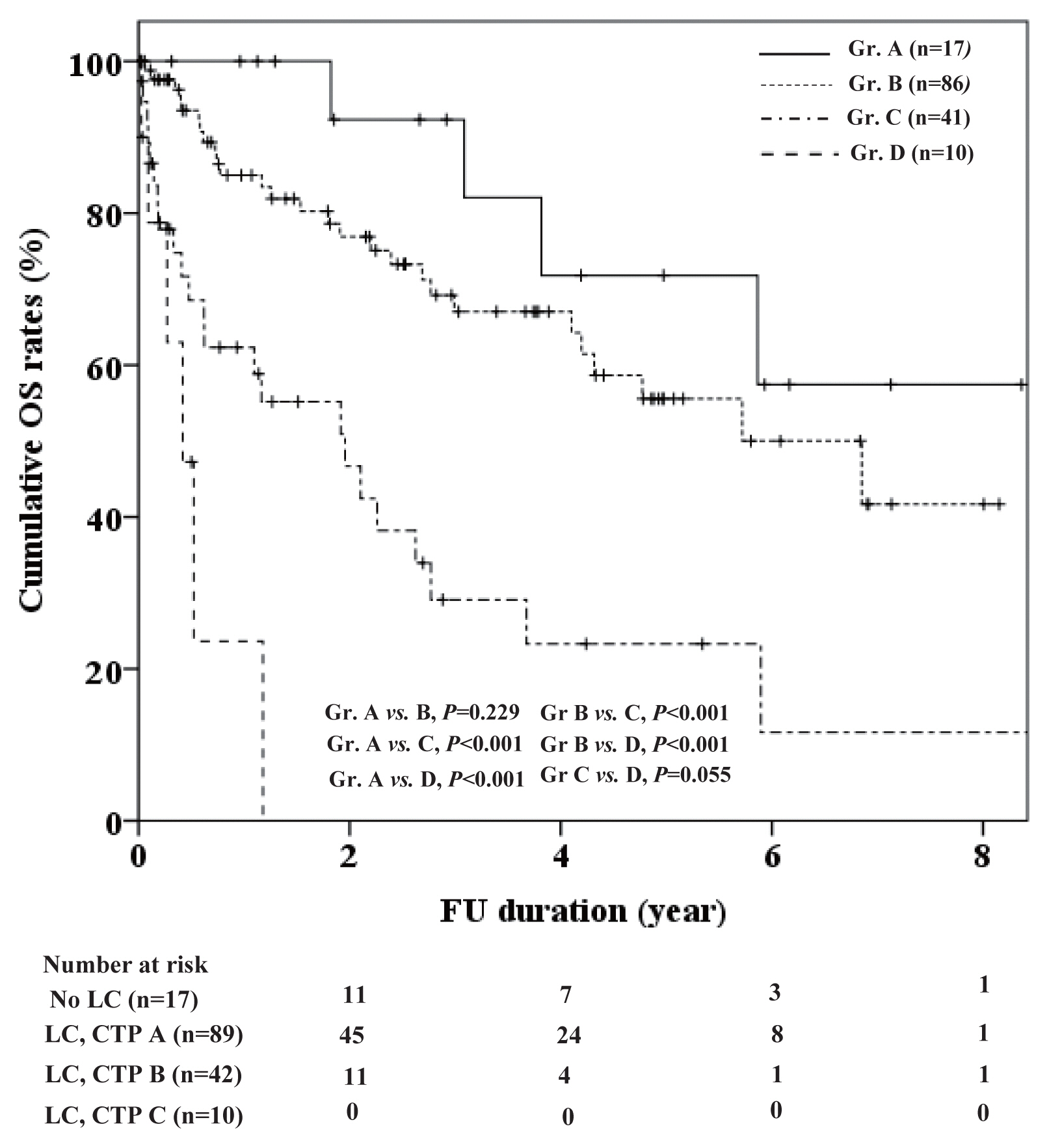
- In order to identify whether OSs were dependent on the remnant liver function rather than LC per se, we compared group OSs according to CTP class between the two groups (Fig. 3). In the non-cirrhotic group, all patients (n=17) were CTP class A (subgroup A), whereas in the cirrhotic group, 86, 41, and 10 patients were of CTP class A (subgroup B), B (subgroup C), and C (subgroup D), respectively. Cumulative OSs of these 4 subgroups were compared. Between the subgroups A and B, their cumulative OSs were not significantly different (P =0.229). The cumulative OS of the subgroup A was better than those of the subgroups C (P <0.001) and D (P <0.001), respectively, and the cumulative OS of the subgroup B was also better than those of the subgroups C (P <0.001) and D (P <0.001), respectively. The cumulative OS of the subgroup C tended to be higher than that of the subgroup D (P =0.055).
- 4. Predictors of OS in HCV-associated HCC patients
- Mutivariate analysis showed that serum AST (HR 1.01 [CI, 1.00–1.01], P =0.003), serum AFP (HR 1.01 [CI, 1.00–1.01], P =0.016), LC with CTP class B (HR 5.24 [CI, 1.62–16.92], P =0.006), LC with CTP class C (HR 21.79 [CI, 4.27–111.39], P <0.001), and a history of AVT (HR 0.25 [CI, 0.07–0.82], P =0.022), were significantly associated with the prognosis of HCV-associated HCC patients (Table 3).
RESULTS
- In this study, among 154 HCV-associated HCC patients, only 17 (11.0%) had a non-cirrhotic liver, and all 17 had well preserved liver function (CTP class A). For these 17 patients, the proportion of males, median platelet count, and median albumin level were significantly higher than in the cirrhotic group, and 12 (70.6%) had BCLC A staged HCC. However, tumor number and median tumor sizes were not significantly different for HCV-associated HCC patients with or without LC. OS was significantly greater in the non-cirrhotic group, but not between patients of CTP class A in the two patient groups. Furthermore, the OSs of HCV-associated HCC patients were better for patients of CTP class A, regardless of LC, than for cirrhotic patients of CTP class B or C. Multivariable analyses showed serum AST, AFP, CTP class B, CTP class C, and a history of AVT were significantly associated with OS in our 154 study subjects.
- HCC usually develops in cirrhotic livers, but 5–70% of HCCs have been reported to develop in patients with a non-cirrhotic livers.3,30–32 And, HCV patients without LC are not subject to surveillance according to AASLD or European Association for the Study of the Liver guideline,22,33 but are subject to surveillance according to Korean Liver Cancer Association-National Cancer Center guideline.34 Moreover, the incidence of HCC in patients with a non-cirrhotic liver depends on the etiology of chronic liver disease.3,30,32 In terms of HCV-associated HCCs, several recent studies have reported that 2–68% of HCCs occur in patients with a non-cirrhotic liver.32,35,36 In the present study, 11.0% of HCV-associated HCC patients were diagnosed without LC, which concurs with previous reports.32,35,36 However, the cost-effectiveness of HCC surveillance for these patients was not evaluated in the present study, and thus, we do not comment on the need for HCC surveillance in these patients. Nonetheless, our findings caution that HCV-associated HCC occurs uncommonly in the absence of cirrhosis.
- In order to identify the features of HCV-associated HCC patients without LC and to determine which HCV patients are more likely to develop HCC in the absence of LC, we compared their clinical features with those of HCV-associated HCC patients with LC. Demographically, HCV-associated HCC in a non-cirrhotic liver was more frequently observed in female patients, which is in-line with a previous study,17 and suggests that sex hormones may be associated with the development of HCV-associated HCC in a non-cirrhotic liver. However, the mechanism of HCC carcinogenesis in HCV patients without LC remains unclear. In the present study, 11 (64.7%) of the 17 HCV-associated HCC patients without LC were diagnosed incidentally during a medical examination despite the absence of symptoms. Therefore, although such patients are not eligible for the current HCC surveillance program,28 more attention should be paid to the diagnosis early HCC despite the absence of symptoms in HCV patients without LC.
- In the present study, we evaluated the OS of HCV-associated HCC patients according to the presence of LC, and compared OSs with respect to CTP class in those with or without LC. In a previous Korean study, although an OS difference was observed between HCC patients with or without LC, the relation between OS and the cause of chronic liver disease was not explored, and the majority of subjects enrolled were HBV-associated HCC patients.37 On the other hand, in the present study, we focused on HCV-associated HCC patients, and found that reserved liver functions in CTP class B or C cases with a cirrhotic liver were significantly associated with poorer OS in HCV-associated HCC patients. However, the non-cirrhotic group did not contain any patient of CTP class B or C, and thus, we could not directly compare OSs of CTP class B or C patients with or without LC. Nonetheless, given that serum levels of albumin or PT are correctable in compensated liver, our findings suggest the correction of liver function before anti-HCC treatment in HCV-associated HCC patients may importantly affect patient’s prognosis. In addition, we found OS was significantly better in patients without LC than in those with LC, as expected. However, we need to interpret this results because the numbers of patients without LC and of their event (death) were small as 7 and 4, respectively, and the follow-up period differs significantly between the cirrhotic and non-cirrhotic group. It is a disadvantage of this study.
- The goal of AVT in patients with HCV infection is to eradicate of virus and decrease the incidence of HCV-related complications including HCC development and mortality. In the present study, we sought to investigate the effects of AVT for HCV on the development of HCC in HCV patients with and without LC, but unfortunately, we failed to do so as only 22 patients received AVT. HCC occurred in 4 (20%) cirrhotic patients despite the achievement of SVR, but it did not develop in non-cirrhotic patients with SVR. On the other hand, it has been reported that AVT can improve reserve liver function in HBV-associated HCC patients, and may reduce the recurrence rate or delay HCC progression.38,39 However, the effect of AVT for HCV infection after diagnosis of HCV-associated HCC on OS is not clear. Although several studies have reported risk of HCC development in HCV patients that receive AVT, these study results should be carefully interpreted because liver status at the time of AVT may have confounded the analyses performed in these retrospective, observational studies. Therefore, we suggest a large-scale prospective study be conducted in HCV patients that receive AVT to investigate these issues.
- In the multivariate analysis, BCLC stage was a significant factor for OS of the enrolled patients, but it was not an independent prognostic factor for OS, unexpectedly. This may be confounded by treatment type for HCC or the presence of LC. Despite the very early/early staged HCC (BCLC stage 0/A), some patients received TACE or supportive care in the present study, and their prognosis was not optimistic. Similarly, curative-intended treatment could not an independent prognostic factor for OS, and this may be also confounded by the presence of LC. However, these findings need to be validated using large scaled prospective multicenter studies.
- This study has several limitations. First, selection bias could not be avoided due to the retrospective design of the present study. Moreover, because of its non-randomized nature, the study is subject to the effects of several confounders although it was conducted on only HCV-associated HCC patients to prevent etiologically-related effects. Therefore, large-scale well designed randomized studies are required. Second, we failed to demonstrate the effects of AVT on HCC development in HCV patients with or without LC due to the small number of patients with a history of AVT and the relatively small number of patients in the non-cirrhotic group. However, in view of the fact that the prevalence of HCV-associated HCC without LC has not been well established in HBV-endemic areas, we hope that our results provide useful information for the follow-up of HCV patients in HBV-endemic areas. Third, due to the retrospective design, we could not confirm LC based on pathologic findings in all enrolled patients.
- Summarizing, 11% of HCV-associated HCC patients do not have underlying cirrhotic liver, and all such patients included in this study had well preserved liver function (CTP class A). This suggests that HCV patients without LC may be also at risk of HCC development in HBV-endemic area, such as South Korea. Therefore, the possibility of HCC development in these patients require attention, despite their ineligibilities for the HCC surveillance program. On the other hand, the OSs of HCV-associated HCC patients were better for those of CTP class A, regardless of LC, than cirrhotic patients of CTP class B or C. This finding suggests preserved liver function rather the presence of LC per se is associated with the prognosis of HCV-related HCC patients, and that every effort should be made to preserve liver function in HCV patients.
DISCUSSION
Acknowledgments
ACKNOWLEDGMENTS
-
FINANCIAL SUPPORTS
No financial support was received for this study.
-
AUTHOR CONTRIBUTIONS
J Shin, JH Yu, and YJ Jin were responsible for the concept and design of the study, the acquisition, analysis, and interpretation of data, and drafting of the manuscript. JH Yu and JW Lee helped with data acquisition.
-
Conflicts of Interest
The authors have no conflict of interest to declare.
Article information
| Variable | Total (n=154) | Cirrhotic (n=137, 89.0%) | Non-cirrhotic (n=17, 11.0%) | P-value* |
|---|---|---|---|---|
| Age (years) | 66 (41–87) | 66 (41–87) | 68 (46–85) | 0.463 |
|
|
||||
| Sex (male) | 99 (64.3) | 84 (61.3) | 15 (88.2) | 0.032† |
|
|
||||
| BMI (kg/m2) | 24.2 (13.8–43.3) | 24.3 (13.8–43.3) | 23.2 (15.4–27.0) | 0.027 |
|
|
||||
| DM | 58 (37.7) | 50 (36.5) | 8 (47.1) | 0.397 |
|
|
||||
| HTN | 66 (42.9) | 56 (40.9) | 10 (58.8) | 0.158 |
|
|
||||
| AST (IU/L) | 63 (13–496) | 68 (18–496) | 41 (13–78) | <0.001 |
|
|
||||
| ALT (IU/L) | 35 (8–222) | 35 (8–222) | 31 (12–71) | 0.012 |
|
|
||||
| PLT (×103/uL) | 110 (28–398) | 106 (28–357) | 209 (106–398) | <0.001 |
|
|
||||
| Albumin (mg/dL) | 3.5 (1.5–4.6) | 3.4 (1.5–4.5) | 3.8 (3.2–4.6) | <0.001 |
|
|
||||
| T-bil. (mg/dL) | 1.0 (0.2–16.0) | 1.0 (0.2–16.0) | 0.6 (0.4–2.1) | <0.001 |
|
|
||||
| PT (INR) | 1.2 (0.9–3.8) | 1.2 (0.9–3.8) | 1.1 (0.9–1.5) | 0.001 |
|
|
||||
| CTP (A/B/C) | 103/41/10 (66.9/26.6/6.5) | 86/41/10 (62.8/29.9/7.3) | 17/0/0 (100/0/0) | 0.004† |
|
|
||||
| APRI | 1.41 (0.11–15.91) | 1.68 (0.27–15.91) | 0.46 (0.11–0.91) | 0.002 |
|
|
||||
| FIB-4 | 6.15 (0.70–44.92) | 7.33 (1.14–44.92) | 1.96 (0.7–6.56) | 0.001 |
|
|
||||
| AVT (yes) | 22 (14.3) | 20 (14.6) | 2 (11.8) | 1.000† |
| Drugs (IFN/DAA) | 20/2 (1.3/85.7) | 18/2 (90.0/10.0) | 2/0 (100/0) | 1.000† |
| SVR (+, yes/no) | 4/18 (18.2/81.8) | 4/16 (20/80) | 0/2 (0/100) | 1.000† |
|
|
||||
| AFP (ng/mL) | 36.4 (1.3–6.1×104) | 41.5 (1.3–6.1×104) | 9.2 (2.9–1.9×103) | 0.001 |
|
|
||||
| Tm. characteristics | ||||
| Type (nodular/diffuse) | 149/5 (96.8/3.2) | 132/5 (96.4/3.6) | 17/0 (100/0) | 1.000† |
| Number (1/≥2) | 86/68 (55.8/44.2) | 76/61 (55.5/44.5) | 10/7 (58.8/41.2) | 0.793 |
| Size (cm) | 2.7 (1.0–16.0) | 2.6 (1.0–16.0) | 4.2 (2.1–8.3) | 0.09 |
|
|
||||
| PVT (presence) | 24 (15.6) | 23 (16.8) | 1 (5.9) | 0.475† |
|
|
||||
| Metastasis (presence) | 5 (3.2) | 5 (3.6) | 0 | 1.000† |
|
|
||||
| BCLC stage | ||||
| 0–A/B–D | 94/60 (61/39) | 82/55 (59.9/40.1) | 12/5 (70.6/29.4) | 0.392 |
|
|
||||
| Initial treatment | ||||
| Curative-intent‡ | 30 (19.5) | 25 (18.2) | 5 (29.4) | 0.273 |
|
|
||||
| Initial treatment type | 0.025† | |||
| OP | 12 (7.8) | 8 (5.8) | 4 (23,5) | |
| RFA | 18 (11.7) | 17 (12.4) | 1 (5.9) | |
| TACE | 86 (55.8) | 75 (54.7) | 11 (64.7) | |
| Supportive care | 29 (18.8) | 29 (21.2) | 0 | |
| Transfer | 9 (5.8) | 8 (5.8) | 1 (5.9) | |
|
|
||||
| FU duration (months) | 18 (1–142) | 15 (1–142) | 37.0 (4–100) | 0.019 |
Values are presented as median (range) or number (%) unless otherwise indicated.
BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AST, aspartate aminotransferase; ALT, alanine aminotransferase; PLT, platelet; T-bil, total bilirubin; PT, prothrombin time; INR, international normalized ratio; CTP, Child-Turcotte-Pugh classification; APRI, aminotransferase to platelet ratio index; FIB-4, fibrosis index based on four factors; AVT, antiviral therapy; IFN, interferon; DAA, direct acting antiviral; SVR, sustained virologic response; AFP, alpha-fetoprotein; Tm, tumor; PVT, portal vein thrombosis; BCLC, Barcelona clinic liver cancer; OP, operation; RFA, radiofrequency ablation; TACE, transarterial chemoembolization; FU, follow-up.
* P values were calculated using the t-test, chi-square test, or
† Fisher-exact test;
‡ Curative-intent treatment: operation or radiofrequency ablation.
HCV, hepatitis C virus; HCC, hepatocellular carcinoma; LC, liver cirrhosis; BMI, body mass index; AST, alanine aspartate; ALT, alanine aminotransferase; PLT, platelet; AVT, antiviral therapy; AFP, alpha-fetoprotein; Sx, symptom; PVT, portal vein thrombosis; BCLC, Barcelona Clinical Liver Cancer; UICC, Union for International Cancer Control; Tx, treatment; M, male; OP, operation; RUQ, right upper quadrant; USG, ultrasonography; F, female; LFT, liver function test; RFA, radiofrequency ablation.
Curative-intent treatment: operation or radiofrequency ablation in the present study. Event: death (n=61).
HCV, hepatitis C virus; HCC, hepatocellular carcinoma; HR, hazard ratio; CI, confidence interval; BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; AST, aspartate aminotransferase; ALT, alanine aminotransferase; AFP, Alpha-fetoprotein; LC, liver cirrhosis; CTP, Child-Turcotte-Pugh classification; AVT, antiviral therapy; BCLC, Barcelona Clinic Liver Cancer; Tx, treatment.
- 1. Global Burden of Disease Cancer C. Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 2017;3:524−548.PubMedPMC
- 2. El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012;142:1264−1273.e1.ArticlePubMedPMC
- 3. Trevisani F, Frigerio M, Santi V, Grignaschi A, Bernardi M. Hepatocellular carcinoma in non-cirrhotic liver: a reappraisal. Dig Liver Dis 2010;42:341−347.ArticlePubMed
- 4. Evert M, Dombrowski F. Hepatocellular carcinoma in the non-cirrhotic liver. Pathologe 2008;29:47−52.ArticlePubMedPDF
- 5. Do AL, Wong CR, Nguyen LH, Nguyen VG, Trinh H, Nguyen MH. Hepatocellular carcinoma incidence in noncirrhotic patients with chronic hepatitis B and patients with cirrhosis of all etiologies. J Clin Gastroenterol 2014;48:644−649.ArticlePubMed
- 6. Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, et al. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology 2002;35:1522−1527.ArticlePubMed
- 7. Yang HI, Lu SN, Liaw YF, You SL, Sun CA, Wang LY, et al. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med 2002;347:168−174.ArticlePubMed
- 8. Huo TI, Wu JC, Lee PC, Chau GY, Lui WY, Tsay SH, et al. Seroclearance of hepatitis B surface antigen in chronic carriers does not necessarily imply a good prognosis. Hepatology 1998;28:231−236.ArticlePubMed
- 9. Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology 1997;112:463−472.ArticlePubMed
- 10. Degos F, Christidis C, Ganne-Carrie N, Farmachidi JP, Degott C, Guettier C, et al. Hepatitis C virus related cirrhosis: time to occurrence of hepatocellular carcinoma and death. Gut 2000;47:131−136.ArticlePubMedPMC
- 11. Niederau C, Lange S, Heintges T, Erhardt A, Buschkamp M, Hürter D, et al. Prognosis of chronic hepatitis C: results of a large, prospective cohort study. Hepatology 1998;28:1687−1695.ArticlePubMed
- 12. Lok AS, Seeff LB, Morgan TR, di Bisceglie AM, Sterling RK, Curto TM, et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology 2009;136:138−148.ArticlePubMed
- 13. Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of hepatocarcinogenesis by interferon therapy. Ann Intern Med 1999;131:174−181.ArticlePubMed
- 14. Bizollon T, Ahmed SN, Radenne S, Chevallier M, Chevallier P, Parvaz P, et al. Long term histological improvement and clearance of intrahepatic hepatitis C virus RNA following sustained response to interferon-ribavirin combination therapy in liver transplanted patients with hepatitis C virus recurrence. Gut 2003;52:283−287.ArticlePubMedPMC
- 15. Chu CY, Cheng CH, Chen HL, Lin IT, Wu CH, Lee YK, et al. Long-term histological change in chronic hepatitis C patients who had received peginterferon plus ribavirin therapy with sustained virological response. J Formos Med Assoc 2019;118:1129−1137.ArticlePubMed
- 16. Conti F, Buonfiglioli F, Scuteri A, Crespi C, Bolondi L, Caraceni P, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol 2016;65:727−733.ArticlePubMed
- 17. Albeldawi M, Soliman M, Lopez R, Zein NN. Hepatitis C virus-associated primary hepatocellular carcinoma in non-cirrhotic patients. Dig Dis Sci 2012;57:3265−3270.ArticlePubMed
- 18. Nash KL, Woodall T, Brown AS, Davies SE, Alexander GJ. Hepatocellular carcinoma in patients with chronic hepatitis C virus infection without cirrhosis. World J Gastroenterol 2010;16:4061−4065.ArticlePubMedPMC
- 19. Schütte K, Schulz C, Poranzke J, Antweiler K, Bornschein J, Bretschneider T, et al. Characterization and prognosis of patients with hepatocellular carcinoma (HCC) in the non-cirrhotic liver. BMC Gastroenterol 2014;14:117. ArticlePubMedPMC
- 20. Yoo SH, Kwon JH, Nam SW, Kim HY, Kim CW, You CR, et al. Early development of de novo hepatocellular carcinoma after direct-acting agent therapy: comparison with pegylated interferon-based therapy in chronic hepatitis C patients. J Viral Hepat 2018;25:1189−1196.ArticlePubMed
- 21. Ogawa E, Furusyo N, Nomura H, Dohmen K, Higashi N, Takahashi K, et al. Short-term risk of hepatocellular carcinoma after hepatitis C virus eradication following direct-acting anti-viral treatment. Aliment Pharmacol Ther 2018;47:104−113.ArticlePubMed
- 22. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018;68:723−750.ArticlePubMed
- 23. Bruix J, Castells A, Bosch J, Feu F, Fuster J, Garcia-Pagan JC, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996;111:1018−1022.ArticlePubMed
- 24. Di Lelio A, Cestari C, Lomazzi A, Beretta L. Cirrhosis: diagnosis with sonographic study of the liver surface. Radiology 1989;172:389−392.ArticlePubMed
- 25. Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet 2014;383:1749−1761.ArticlePubMed
- 26. Lin ZH, Xin YN, Dong QJ, Wang Q, Jiang XJ, Zhan SH, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology 2011;53:726−736.ArticlePubMed
- 27. Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006;43:1317−1325.ArticlePubMed
- 28. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020−1022.ArticlePubMedPMC
- 29. Leung C, Yeoh SW, Patrick D, Ket S, Marion K, Gow P, et al. Characteristics of hepatocellular carcinoma in cirrhotic and non-cirrhotic non-alcoholic fatty liver disease. World J Gastroenterol 2015;21:1189−1196.ArticlePubMedPMC
- 30. Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 2004;127(5 Suppl 1): S35−S50.ArticlePubMed
- 31. European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908−943.ArticlePubMed
- 32. Trevisani F, D’Intino PE, Caraceni P, Pizzo M, Stefanini GF, Mazziotti A, et al. Etiologic factors and clinical presentation of hepatocellular carcinoma. Differences between cirrhotic and noncirrhotic Italian patients. Cancer 1995;75:2220−2232.ArticlePubMed
- 33. European Association for the Study of the Liver, European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182−236.ArticlePubMed
- 34. Kim TH, Kim SY, Tang A, Lee JM. Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma: 2018 update. Clin Mol Hepatol 2019;25:245−263.ArticlePubMedPMC
- 35. Bralet MP, Regimbeau JM, Pineau P, Dubois S, Loas G, Degos F, et al. Hepatocellular carcinoma occurring in nonfibrotic liver: epidemiologic and histopathologic analysis of 80 French cases. Hepatology 2000;32:200−204.ArticlePubMed
- 36. Kumar M, Kumar R, Hissar SS, Saraswat MK, Sharma BC, Sakhuja P, et al. Risk factors analysis for hepatocellular carcinoma in patients with and without cirrhosis: a case-control study of 213 hepatocellular carcinoma patients from India. J Gastroenterol Hepatol 2007;22:1104−1111.ArticlePubMed
- 37. Shim CW, Park JW, Kim SH, Kim JS, Kim BH, Kim SH, et al. Noncirrhotic hepatocellular carcinoma: etiology and occult hepatitis B virus infection in a hepatitis B virus-endemic area. Therap Adv Gastroenterol 2017;10:529−536.ArticlePubMedPMC
- 38. Yin J, Li N, Han Y, Xue J, Deng Y, Shi J, et al. Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: a two-stage longitudinal clinical study. J Clin Oncol 2013;31:3647−3655.ArticlePubMed
- 39. Huang G, Lau WY, Wang ZG, Pan ZY, Yuan SX, Shen F, et al. Antiviral therapy improves postoperative survival in patients with hepatocellular carcinoma: a randomized controlled trial. Ann Surg 2015;261:56−66.ArticlePubMed
References
Figure & Data
References
Citations

- Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma
Jun Il Kim, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park, Jeong-Ju Yoo
Digestive Diseases and Sciences.2024; 69(3): 1055. CrossRef

 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION
 PubReader
PubReader ePub Link
ePub Link Download Citation
Download Citation

 Follow JLC on Twitter
Follow JLC on Twitter