Search
- Page Path
- HOME > Search
Review Article
- Non-alcoholic fatty liver disease-related hepatocellular carcinoma
- Darine Daher, Karim Seif El Dahan, Amit G. Singal
- J Liver Cancer. 2023;23(1):127-142. Published online February 9, 2023
- DOI: https://doi.org/10.17998/jlc.2022.12.30

- 3,314 Views
- 173 Downloads
- 7 Citations
-
 Abstract
Abstract
 PDF
PDF - Non-alcoholic fatty liver disease (NAFLD), one of the most common causes of liver disease, is an increasingly common cause of hepatocellular carcinoma (HCC). Several demographic, clinical, and genetic factors contribute to HCC risk in NAFLD patients, which may inform risk stratification scores. Proven efficacious approaches to primary prevention approach in patients with non-viral liver disease remain an area of need. Semi-annual surveillance is associated with improved early tumor detection and reduced HCC-related mortality; however, patients with NAFLD have several challenges to effective surveillance, including under-recognition of at-risk patients, low surveillance utilization in clinical practice, and lower sensitivity of current tools for early-stage HCC detection. Treatment decisions are best made in a multidisciplinary fashion and are informed by several factors including tumor burden, liver dysfunction, performance status, and patient preferences. Although patients with NAFLD often have larger tumor burden and increased comorbidities compared to counterparts, they can achieve similar post-treatment survival with careful patient selection. Therefore, surgical therapies continue to provide a curative treatment option for patients diagnosed at an early stage. Although there has been debate about the efficacy of immune checkpoint inhibitors in patients with NAFLD, current data are insufficient to change treatment selection based on liver disease etiology.
-
Citations
Citations to this article as recorded by- Overnutrition and Lipotoxicity: Impaired Efferocytosis and Chronic Inflammation as Precursors to Multifaceted Disease Pathogenesis
Vivek Mann, Alamelu Sundaresan, Shishir Shishodia
Biology.2024; 13(4): 241. CrossRef - Risk of Hepatocellular Carcinoma by Steatotic Liver Disease and Its Newly Proposed Subclassification
Byeong Geun Song, Aryoung Kim, Myung Ji Goh, Wonseok Kang, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Dong Hyun Sinn
Liver Cancer.2024; : 1. CrossRef - Smoking Increases the Risk of Hepatocellular Carcinoma and Cardiovascular Disease in Patients with Metabolic-Associated Fatty Liver Disease
Jeong-Ju Yoo, Man Young Park, Eun Ju Cho, Su Jong Yu, Sang Gyune Kim, Yoon Jun Kim, Young Seok Kim, Jung-Hwan Yoon
Journal of Clinical Medicine.2023; 12(9): 3336. CrossRef - Reply: Validation of MELD 3.0 scoring system in East Asian patients with cirrhosis awaiting liver transplantation
Jeong-Ju Yoo, Sang Gyune Kim
Liver Transplantation.2023; 29(11): E38. CrossRef - Unraveling the Janus-Faced Role of Autophagy in Hepatocellular Carcinoma: Implications for Therapeutic Interventions
Thi Ha Nguyen, Tuan Minh Nguyen, Dinh Thi Minh Ngoc, Taesik You, Mi Kyung Park, Chang Hoon Lee
International Journal of Molecular Sciences.2023; 24(22): 16255. CrossRef - Comparative Analysis of Atezolizumab Plus Bevacizumab and Hepatic Artery Infusion Chemotherapy in Unresectable Hepatocellular Carcinoma: A Multicenter, Propensity Score Study
Ji Kim, Hee-Chul Nam, Chang-Wook Kim, Hee Cho, Jae-Sung Yoo, Ji Han, Jeong Jang, Jong Choi, Seung Yoon, Hyun Yang, Si Bae, Suho Kim, Jung Oh, Ho Chun, Chang Jeon, Jaegyoon Ahn, Pil Sung
Cancers.2023; 15(17): 4233. CrossRef - A nationwide study on the current treatment status and natural prognosis of hepatocellular carcinoma in elderly
Jeong-Ju Yoo, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park
Scientific Reports.2023;[Epub] CrossRef
- Overnutrition and Lipotoxicity: Impaired Efferocytosis and Chronic Inflammation as Precursors to Multifaceted Disease Pathogenesis

Original Articles
- A Survey of Liver Cancer Specialists’ Views on the National Liver Cancer Screening Program in Korea
- Won Sohn, Young-Sun Lee, Jae Geun Lee, Jihyun An, Eun Sun Jang, Dong Ho Lee, Dong Hyun Sinn
- J Liver Cancer. 2020;20(1):53-59. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.53
- 4,327 Views
- 133 Downloads
- 5 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
s: To reduce the cancer burden, the Korean government initiated the National Cancer Control Plan including the National Liver Cancer Screening Program (NLCSP). Ultrasonography examinations and α-fetoprotein tests at six-month intervals are currently offered for high-risk individuals. High-risk individuals are identified by reviewing the National Health Insurance Service claims data for medical use for the past two years using International Classification of Diseases Codes for specific liver disease. We surveyed the attitudes and opinions towards the NLCSP to understand the issues surrounding the NLCSP in Korea.
Methods
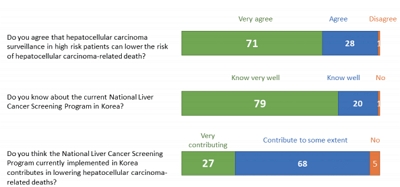
Altogether, 90 Korean Liver Cancer Association members participated in online and offline surveys between November and December 2019.
Results
Approximately one-quarter (27%) of the survey participants rated the NLCSP as very contributing and about two-thirds (68%) as contributing to some extent toward reducing hepatocellular carcinoma (HCC)-related deaths in Korea. Most (87.8%) responded that the current process of identifying high-risk individuals needs improvement. Many (78.9%) were concerned that the current process identifies individuals who use medical services and paradoxically misses those who do not. When asked for the foremost priority for improvement, solving ‘duplication issues between the NLCSP and private clinic HCC screening practices’ was the most commonly selected choice (23.3%).
Conclusions
The survey participants positively rated the role of the NLCSP in reducing liver cancer deaths. However, many participants rated the NCLSP as needing improvement in all areas. This survey can be a relevant resource for future health policy decisions regarding the NLCSP in Korea. -
Citations
Citations to this article as recorded by- Potential role of Fibrosis‐4 score in hepatocellular carcinoma screening: The Kangbuk Samsung Health Study
Sujeong Shin, Won Sohn, Yoosoo Chang, Yoosun Cho, Min‐Jung Kwon, Sarah H. Wild, Christopher D. Byrne, Seungho Ryu
Hepatology Research.2024;[Epub] CrossRef - Clinical practice guideline and real-life practice in hepatocellular carcinoma: A Korean perspective
Myung Ji Goh, Dong Hyun Sinn, Jong Man Kim, Min Woo Lee, Dong Ho Hyun, Jeong Il Yu, Jung Yong Hong, Moon Seok Choi
Clinical and Molecular Hepatology.2023; 29(2): 197. CrossRef - Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, J
Journal of Liver Cancer.2023; 23(1): 189. CrossRef - Selecting the Target Population for Screening of Hepatic Fibrosis in Primary Care Centers in Korea
Huiyul Park, Eileen L. Yoon, Mimi Kim, Seon Cho, Jung-Hwan Kim, Dae Won Jun, Eun-Hee Nah
Journal of Clinical Medicine.2022; 11(6): 1474. CrossRef - Fibrosis Burden of Missed and Added Populations According to the New Definition of Metabolic Dysfunction-Associated Fatty Liver
Huiyul Park, Eileen L. Yoon, Mimi Kim, Jung-Hwan Kim, Seon Cho, Dae Won Jun, Eun-Hee Nah
Journal of Clinical Medicine.2021; 10(19): 4625. CrossRef
- Potential role of Fibrosis‐4 score in hepatocellular carcinoma screening: The Kangbuk Samsung Health Study

- Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
- Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
- J Liver Cancer. 2019;19(1):30-37. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.30
- 4,466 Views
- 95 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: The National Liver Cancer Screening Program (NLCSP) has been implemented for the past 15 years in Korea. However, the actual clinical experience in Korea is inconsistent with the expectations of the hepatocellular carcinoma (HCC) surveillance program. To evaluate the actual clinical situation of HCC diagnoses, we investigated disease severity in patients with HCC and the diagnostic environment.
Methods
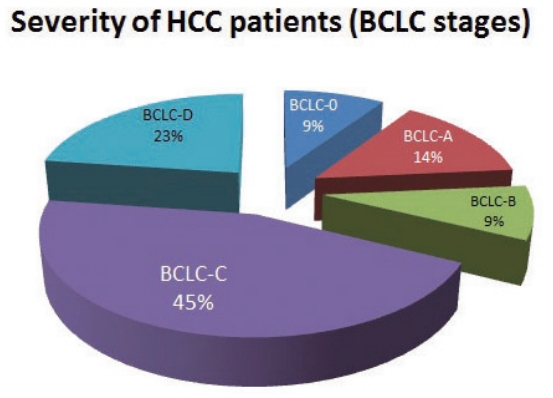
From January 2011 to December 2015, all patients who were diagnosed with HCC in a single secondary hospital in Daejeon city were retrospectively enrolled in this study. Severity of HCC was evaluated according to the Barcelona Clinic Liver Cancer (BCLC) staging system.
Results
Over the course of 5 years, 298 participants were enrolled. The mean age of participants was 64.0 years. Positive hepatitis B surface antigen was confirmed in 134 patients (45.0%), 35 patients (11.7%) tested positive for anti-hepatitis C virus antibody, and 93 patients (32.2%) had more than 40 g/day of alcohol consumption. The proportions of patients according to BCLC stages were as follows: BCLC-0, 28 patients (9.4%); BCLC-A, 42 patients (14.1%); BCLC-B, 26 patients (8.7%); BCLC-C, 134 patients (45.0%); and BCLC-D, 68 patients (22.8%). The diagnostic environments were as follows: 19 patients were in the NLCSP group (6.4%), 114 in the group with presenting signs (38.3%), 110 in the regular outpatient care group (36.9%), and 55 patients in the incidental diagnosis group (18.5%).
Conclusions
Most patients (67.8%) had advanced stage HCC at diagnosis, and curative treatment was not indicated due to the severity disease. Thus, the actual situation is far worse than the theoretical expectation of HCC surveillance, suggesting that many high-risk patients for HCC are missed in surveillance. -
Citations
Citations to this article as recorded by- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis
Wojciech Książek, Filip Turza, Paweł Pławiak
International Journal for Numerical Methods in Biomedical Engineering.2022;[Epub] CrossRef - Imaging Modalities for Hepatocellular Carcinoma Surveillance: Expanding Horizons beyond Ultrasound
Hyo Jung Park, So Yeon Kim
Journal of Liver Cancer.2020; 20(2): 99. CrossRef
- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis

- Incidence of Primary Liver Cancer in Subjects with Chronic Hepatitis B in Korean National Liver Cancer Screening Program
- In Seung Choi, Chi Hyuck Oh, So Young Park, Sung Eun Ahn, Seong Jin Park, Hyun Rim Choi, Byung-Ho Kim, Jae-Jun Shim
- J Liver Cancer. 2017;17(2):136-143. Published online September 30, 2017
- DOI: https://doi.org/10.17998/jlc.17.2.136
- 3,940 Views
- 49 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: To optimize efficacy of National Liver Cancer Screening Program (NLCSP) for subjects with chronic hepatitis B (CHB), it is needed to know the incidence of liver cancer and its predisposing factors in the program.
Methods
From January 2010 to December 2014, all the hepatitis B surface antigen (HBsAg) positive participants who received at least two or more abdominal ultrasonography under NLCSP were retrospectively enrolled in a single tertiary hospital. Annual incidence of primary liver cancer was calculated and related clinical factors were investigated.
Results
During 5 years, 541 subjects were enrolled. Mean age was 53 years old and 292 subjects (54%) were receiving antiviral agents. Liver cirrhosis (LC) was diagnosed in 212 (39.2%). Mean follow-up time was 2.36 years and 15 hepatocellular carcinoma and 1 intrahepatic cholangiocarcinoma were diagnosed. Annual incidence of primary liver cancer was 9.8 per 1,000 patient year. Cumulative incidence at 1, 3, and 5 year was 0.6%, 2.6%, and 6.4%, respectively. In multivariate analyses, LC (hazard ratio [HR] 8.74, 95% confidence interval [CI] 1.97–38.71, P=0.024), age (HR 1.08, 95% CI 1.01–1.15, P=0.024) were significantly associated with cancer development.
Conclusions
Despite of high rate of oral antiviral therapy, incidence of primary liver cancer is not low in CHB patients in Korea. Old age and presence of LC are independently associated with higher risk of cancer development during surveillance. This study could be used as baseline data for quality control of NLCSP. -
Citations
Citations to this article as recorded by- Effectiveness of Hepatocellular Carcinoma Surveillance and an Optimal Surveillance Interval: Nationwide Cohort of Korea
Heejin Bae, Sang Ah Lee, Jong Won Choi, Shin Hye Hwang, Sumi Park, Mi-Suk Park
Yonsei Medical Journal.2021; 62(8): 758. CrossRef - A Survey of Liver Cancer Specialists’ Views on the National Liver Cancer Screening Program in Korea
Won Sohn, Young-Sun Lee, Jae Geun Lee, Jihyun An, Eun Sun Jang, Dong Ho Lee, Dong Hyun Sinn
Journal of Liver Cancer.2020; 20(1): 53. CrossRef - Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
Journal of Liver Cancer.2019; 19(1): 30. CrossRef
- Effectiveness of Hepatocellular Carcinoma Surveillance and an Optimal Surveillance Interval: Nationwide Cohort of Korea


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev


 Follow JLC on Twitter
Follow JLC on Twitter