Search
- Page Path
- HOME > Search
Original Articles
- Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
- Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
- J Liver Cancer. 2019;19(1):30-37. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.30
- 4,466 Views
- 95 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: The National Liver Cancer Screening Program (NLCSP) has been implemented for the past 15 years in Korea. However, the actual clinical experience in Korea is inconsistent with the expectations of the hepatocellular carcinoma (HCC) surveillance program. To evaluate the actual clinical situation of HCC diagnoses, we investigated disease severity in patients with HCC and the diagnostic environment.
Methods
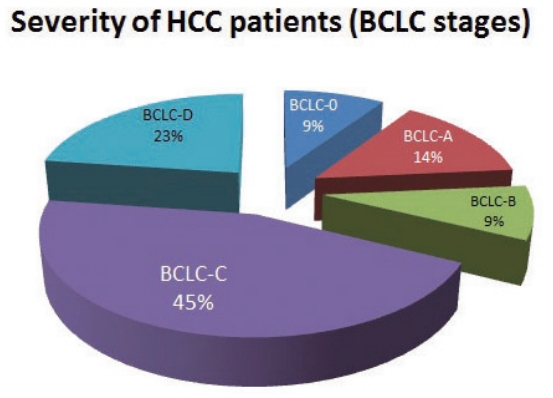
From January 2011 to December 2015, all patients who were diagnosed with HCC in a single secondary hospital in Daejeon city were retrospectively enrolled in this study. Severity of HCC was evaluated according to the Barcelona Clinic Liver Cancer (BCLC) staging system.
Results
Over the course of 5 years, 298 participants were enrolled. The mean age of participants was 64.0 years. Positive hepatitis B surface antigen was confirmed in 134 patients (45.0%), 35 patients (11.7%) tested positive for anti-hepatitis C virus antibody, and 93 patients (32.2%) had more than 40 g/day of alcohol consumption. The proportions of patients according to BCLC stages were as follows: BCLC-0, 28 patients (9.4%); BCLC-A, 42 patients (14.1%); BCLC-B, 26 patients (8.7%); BCLC-C, 134 patients (45.0%); and BCLC-D, 68 patients (22.8%). The diagnostic environments were as follows: 19 patients were in the NLCSP group (6.4%), 114 in the group with presenting signs (38.3%), 110 in the regular outpatient care group (36.9%), and 55 patients in the incidental diagnosis group (18.5%).
Conclusions
Most patients (67.8%) had advanced stage HCC at diagnosis, and curative treatment was not indicated due to the severity disease. Thus, the actual situation is far worse than the theoretical expectation of HCC surveillance, suggesting that many high-risk patients for HCC are missed in surveillance. -
Citations
Citations to this article as recorded by- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis
Wojciech Książek, Filip Turza, Paweł Pławiak
International Journal for Numerical Methods in Biomedical Engineering.2022;[Epub] CrossRef - Imaging Modalities for Hepatocellular Carcinoma Surveillance: Expanding Horizons beyond Ultrasound
Hyo Jung Park, So Yeon Kim
Journal of Liver Cancer.2020; 20(2): 99. CrossRef
- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis

- Incidence of Primary Liver Cancer in Subjects with Chronic Hepatitis B in Korean National Liver Cancer Screening Program
- In Seung Choi, Chi Hyuck Oh, So Young Park, Sung Eun Ahn, Seong Jin Park, Hyun Rim Choi, Byung-Ho Kim, Jae-Jun Shim
- J Liver Cancer. 2017;17(2):136-143. Published online September 30, 2017
- DOI: https://doi.org/10.17998/jlc.17.2.136
- 3,940 Views
- 49 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: To optimize efficacy of National Liver Cancer Screening Program (NLCSP) for subjects with chronic hepatitis B (CHB), it is needed to know the incidence of liver cancer and its predisposing factors in the program.
Methods
From January 2010 to December 2014, all the hepatitis B surface antigen (HBsAg) positive participants who received at least two or more abdominal ultrasonography under NLCSP were retrospectively enrolled in a single tertiary hospital. Annual incidence of primary liver cancer was calculated and related clinical factors were investigated.
Results
During 5 years, 541 subjects were enrolled. Mean age was 53 years old and 292 subjects (54%) were receiving antiviral agents. Liver cirrhosis (LC) was diagnosed in 212 (39.2%). Mean follow-up time was 2.36 years and 15 hepatocellular carcinoma and 1 intrahepatic cholangiocarcinoma were diagnosed. Annual incidence of primary liver cancer was 9.8 per 1,000 patient year. Cumulative incidence at 1, 3, and 5 year was 0.6%, 2.6%, and 6.4%, respectively. In multivariate analyses, LC (hazard ratio [HR] 8.74, 95% confidence interval [CI] 1.97–38.71, P=0.024), age (HR 1.08, 95% CI 1.01–1.15, P=0.024) were significantly associated with cancer development.
Conclusions
Despite of high rate of oral antiviral therapy, incidence of primary liver cancer is not low in CHB patients in Korea. Old age and presence of LC are independently associated with higher risk of cancer development during surveillance. This study could be used as baseline data for quality control of NLCSP. -
Citations
Citations to this article as recorded by- Effectiveness of Hepatocellular Carcinoma Surveillance and an Optimal Surveillance Interval: Nationwide Cohort of Korea
Heejin Bae, Sang Ah Lee, Jong Won Choi, Shin Hye Hwang, Sumi Park, Mi-Suk Park
Yonsei Medical Journal.2021; 62(8): 758. CrossRef - A Survey of Liver Cancer Specialists’ Views on the National Liver Cancer Screening Program in Korea
Won Sohn, Young-Sun Lee, Jae Geun Lee, Jihyun An, Eun Sun Jang, Dong Ho Lee, Dong Hyun Sinn
Journal of Liver Cancer.2020; 20(1): 53. CrossRef - Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
Journal of Liver Cancer.2019; 19(1): 30. CrossRef
- Effectiveness of Hepatocellular Carcinoma Surveillance and an Optimal Surveillance Interval: Nationwide Cohort of Korea


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev


 Follow JLC on Twitter
Follow JLC on Twitter